Do you want to reduce your COVID-19 risk? Research says sleep more.
OBSERVATIONS ABOUT SLEEP and its health benefits date back at least 2,000 years.
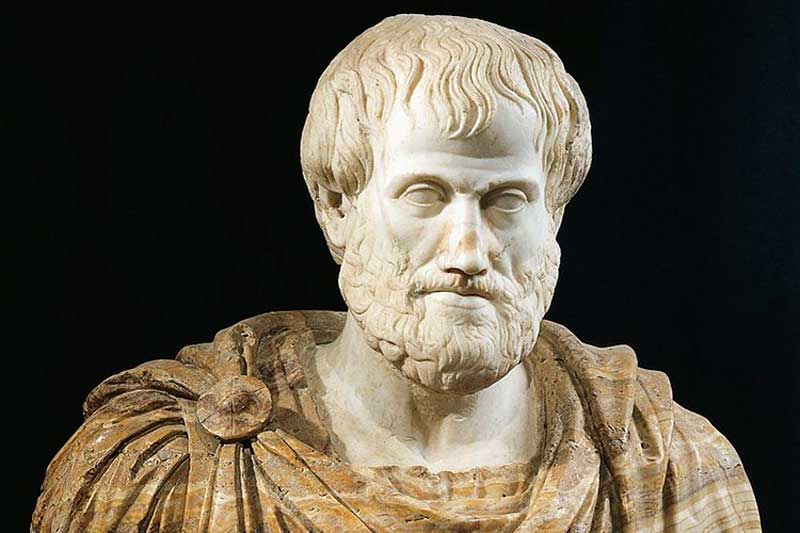
Aristotle’s publication On Sleep and Sleeplessness in 350 B.C. suggested that digestion in the stomach produces hot vapors that lead to sleep, and that people with fevers experience something similar, driving them to snooze to help the healing process.
While the vapors idea did not pan out, decades of scientific evidence show that sleep is a solid way to bolster the immune system against colds, influenza, and respiratory infections. That work suggests that sleep may be a powerful tool to fight the pandemic—and not just by reducing the likelihood or severity of infections. Sleep may ultimately boost the effectiveness of COVID-19 vaccines when they become available, and a flurry of studies are underway measuring how much of a health buffer we gain against the coronavirus by hitting the sack.
“We have a lot of evidence that if you have an adequate amount of sleep, you definitely can help to prevent or fight any kind of infection,” says Monika Haack, a psychoneuroimmunologist at Harvard Medical School in Boston. “How many deaths can you prevent if you sleep properly, or how much less is the severity of your symptoms? I think that needs more research.”
Until a vaccine is available for COVID-19, the key to avoiding COVID-19 is reducing one’s risk of infection as much as possible. As new data roll in on sleep and this disease, scientists hope to better elucidate the complex workings of the immune system, while also providing clearer guidelines on how to use sleep as a weapon to stave off the pandemic.
The sleep-infection connection
Humans aren’t the only animals to benefit from sleep. Grisly studies from the late 1800s showed that when dogs and rats are completely deprived of sleep, the animals die within a couple of weeks. For people, chronic sleep deprivation has long-term consequences, too, raising risks for type 2 diabetes, cardiovascular disease, dementia, and depression. Some of those chronic conditions are among the risk factors that increase susceptibility to COVID-19.
When tired, people also tend to take more risks, says Lt. Col. Vincent Capaldi, chief of the Department of Behavioral Biology at the Walter Reed Army Institute of Research’s Center for Military Psychiatry and Neuroscience Research in Silver Spring, Maryland. Sleep loss is particularly common among soldiers, and Walter Reed devotes a whole research center to understanding how staying awake too long impacts one’s ability to think and function.
“You’re putting yourself at increased risk of making an error when it comes to protecting yourself when you are sleep deprived,” Colonel Capaldi says. For the general public, that could manifest as being sloppy or forgetful about wearing masks, adding an extra stressor on the immune system.
Growing evidence also shows that sleep deprivation impairs a person’s ability to fight off a disease once they are infected. In a number of studies, people with sleep disorders, people who catch less than five or six hours of shut-eye per night, and people with low levels of sleep efficiency (the percentage of time spent snoozing during the night) report higher rates of respiratory illnesses, head colds, and related ills and even COVID-19.
Sleeping more than 10 hours a night has been linked with higher rates of illness, but experts say that extra snoozing probably doesn’t cause people to become sick. Instead, underlying health conditions that include depression may cause oversleeping. Or conditions such as diabetes or sleep apnea may cause poor sleep quality, leading to long nights with less overall sleep.
Some studies have even tracked the road directly from sleep to illness, as opposed to simply seeing if sleep is associated with infection. Researchers at the University of California, San Francisco, and Carnegie Mellon University in Pittsburgh recruited 164 healthy adults to wear research-grade Fitbit-type devices that tracked their sleep habits for a week. Then, they went into the lab, where researchers squirted drops of rhinovirus (the common cold) up to their noses before quarantining them in a hotel for five days.
The virus was equally likely to invade people’s bodies and replicate, regardless of how much sleep they got, the team reported in 2015. But those who slept less than six hours were 4.5 times more likely to develop cold symptoms, compared to people who slept more than seven hours a night. Rhinoviruses are good corollaries for coronaviruses; for one thing, the immune responses to both appear to be similar, says study co-author Aric Prather, a psychoneuroimmunologist at UCSF.
Sleep and related health consequences are also intertwined with the types of social inequities that the pandemic has laid bare. In a separate study published in 2017, Prather and colleagues pooled data on 732 people from three rhinovirus studies and found a similar relationship, with a twist.
Only people who ranked themselves low on measures of socioeconomic status (based on questions about income, education, and jobs) showed an increased likelihood of getting colds after being sleep deprived. These disparities are mirrored in the infection rates for the SARS-CoV-2 virus. Part of the problem is that not everyone can get enough sleep, given that people in lower-income brackets often work multiple jobs or overnight shifts. (Millennials and Gen Z are spreading coronavirus—but not because of parties and bars.)
“It’s really a social justice issue around people’s ability to get the sleep they need,” Prather says. “All of those things drive these sleep disorders and map onto disparities in a bunch of outcomes, and likely on to COVID as well.”
Sleep and the immune system
Studies that manipulate sleep—either depriving people of it or increasing how much they get—are starting to untangle why there is such an intricate relationship between sleep and the immune system.
“We know that you need sleep to fight infections,” Harvard’s Haack says. “But how exactly it works, I think there’s still a lot of work to do.”
In a 2019 study, Haack and colleagues listed more than three dozen ways that various immune-system players vary based on sleep changes.
For instance, T cells are part of the immune system and are often described as the soldiers that fight infections. During sleep, according to studies by German researchers, T cells normally move out of the blood and likely into lymph nodes, where they conduct surveillance for invading pathogens, Haack says. But just one night of sleep deprivation, studies show, is enough to keep T cells circulating in the blood, making them less able to learn about and respond to invading viruses. When the body is denied sleep, T cells also become less able to interact with virus-infected cells, reducing their power to fight the infection.
Cytokines, a category of inflammatory molecules connected to the pandemic, are also a major focus of research on sleep and immunity. Pro-inflammatory cytokines normally help organize an immune response to infections, triggering other cells to come fight, says Sheldon Cohen, a psychoneuroimmunologist at Carnegie Mellon University. But the production of too many of these molecules adds up to a cytokine storm, an overreaction associated with severe and fatal cases of COVID-19. In studies of colds and influenza, infected people with poor sleep show worse symptoms, probably because elevated levels of pro-inflammatory cytokines interfere with T cells and other immune cells.
Cytokines don’t work in isolation but are instead part of creating a balance in the immune system between factors that promote and counteract inflammation. Learning how the process works to influence diseases like COVID-19 is still a work in progress.







